Platelet-Rich Plasma Injections
What is Platelet-Rich Plasma Therapy?
Platelet-Rich Plasma (abbreviated PRP) is a treatment used for a variety of common orthopedic conditions. PRP is a concentration of platelet cells taken from your blood, and these platelets have growth factors that may help in the healing process of chronic injuries. Growth factors are chemicals that signal the body to initiate a healing response. By injecting PRP into areas of an injury, the hope is to stimulate and optimize your body’s ability to heal the chronic conditions. PRP contains a high concentration of platelets, other blood cells important in healing, and growth factors.
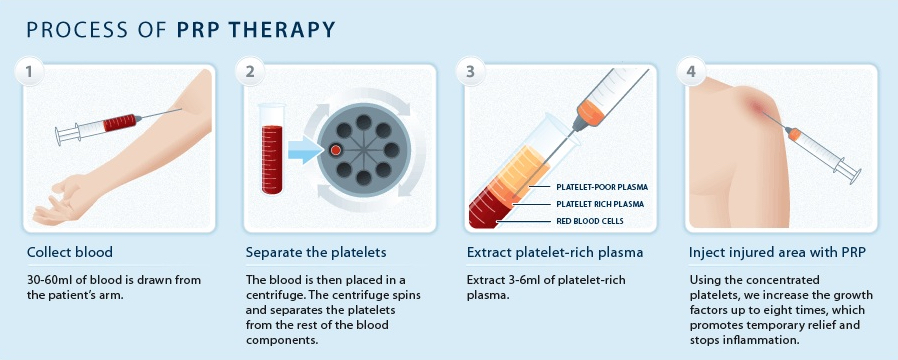
How PRP Is Obtained?
PRP is obtained from the patient who is being treated. Blood is withdrawn from a vein in the patient’s arm and the blood is placed in a centrifuge, a machine that spins at a high speed to separate the different types of blood cells. The physician extracts the platelet-rich portion of the blood, and injects this into the area of injury, jump-starting and significantly strengthening the healing process. There are not just platelets in the concentrated layer of the “spun” blood, but also other important growth factors, plasma, and some red blood cells. Because your own blood is used, there is no risk of transmissible infection and a low risk of an allergic reaction.
PRP is the next-generation injection procedure commonly used in the following conditions:
PRP has been used in operating rooms for several decades to help with wound healing, and to stimulate bone formation in spinal fusion surgery. Recently, PRP has been used in outpatient settings for treatment of common conditions including:
- Tendonitis
- Rotator Cuff Injuries
- ACL Injuries
- Tennis Elbow
- Hair Loss
- Chronic Plantar Fascitis
- Back and Neck Injuries
- And more…